How to Manage Symptoms Type 1 Diabetes and Management Strategies
Type 1 Diabetes is a chronic condition characterized by the body’s inability to produce insulin, a hormone essential for converting glucose into energy. This autoimmune disease can lead to serious health complications if not managed properly. In this article, we will explore the effects of Type 1 diabetes, its symptoms, and effective strategies for management and reduction.
What is Diabetes?
Diabetes is a chronic metabolic disorder characterized by high blood sugar levels over a prolonged period. It occurs when the body either does not produce enough insulin or cannot effectively use the insulin it produces.
Diabetes classified into three types:
- Type 1 Diabetes: An autoimmune condition where the body does not produce insulin.
- Type 2 Diabetes: The more common form, where the body either resists the effects of insulin or doesn’t produce enough to maintain normal glucose levels.
- Gestational Diabetes: A form of diabetes that occurs during pregnancy when the body cannot produce enough insulin.
- Risk Factors: Includes obesity, a family history of diabetes, and being over the age of 25.
- Management: Typically resolves after childbirth but increases the risk of developing Type 2 diabetes later.
What is Type 1 Diabetes?
Type 1 diabetes occurs when the immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas. This typically results in a complete lack of insulin, necessitating lifelong management through insulin therapy and other lifestyle adjustments. Although it can develop at any age, it often manifests in childhood or early adulthood.
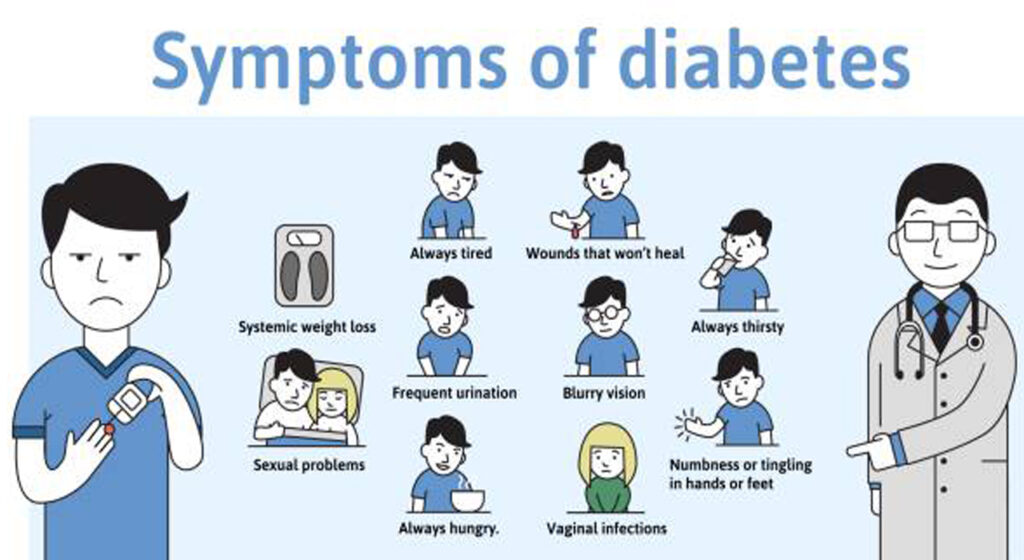
Symptoms of Type 1 Diabetes
Recognizing the symptoms of Type 1 diabetes is crucial for early diagnosis and intervention. Common symptoms include:
- Increased Thirst: Excess glucose in the bloodstream leads to dehydration, causing intense thirst.
- Frequent Urination: High blood sugar levels prompt the kidneys to excrete excess glucose, resulting in frequent urination.
- Extreme Hunger: Despite eating, individuals may feel hungry due to the body’s inability to use glucose for energy.
- Fatigue: The lack of insulin prevents glucose from entering cells, leading to fatigue and weakness.
- Blurred Vision: High blood sugar levels can cause swelling in the eye lenses, impairing vision.
- Slow Healing of Wounds: Elevated glucose levels can affect blood circulation and the body’s healing processes.
- Unexplained Weight Loss: Despite increased hunger and eating, individuals may lose weight due to the body using fat and muscle for energy instead of glucose.
Effects of Type 1 Diabetes on the Body
If not effectively managed, Type 1 diabetes can lead to serious health complications over time:
- Cardiovascular Disease: Increased risk of heart disease and stroke due to damage to blood vessels and nerves.
- Kidney Damage (Diabetic Nephropathy): Chronic high blood sugar can damage the kidneys’ filtering system, potentially leading to kidney failure.
- Nerve Damage (Diabetic Neuropathy): High glucose levels can harm nerves, particularly in the legs and feet, leading to pain and numbness.
- Eye Problems: Increased risk of diabetic retinopathy, cataracts, and glaucoma, which can lead to vision loss.
- Skin Conditions: Higher susceptibility to infections and skin problems.
- Foot Complications: Nerve damage and reduced blood flow can result in severe foot issues, including infections and ulcers.
Management and Reduction Strategies for Type 1 Diabetes
Managing Type 1 diabetes effectively involves a combination of insulin therapy, lifestyle adjustments, and regular monitoring. Here are key strategies:
-
Insulin Therapy
- Types of Insulin: Individuals with Type 1 diabetes require insulin to manage blood sugar levels. This can include:
- Rapid-acting insulin: Used before meals to control postprandial blood sugar spikes.
- Long-acting insulin: Provides a steady level of insulin throughout the day.
- Insulin Delivery Methods: Insulin can be administered via syringes, insulin pens, or insulin pumps, depending on individual preferences and lifestyle.
- Healthy Eating
- Balanced Diet: Focus on a diet rich in whole grains, lean proteins, healthy fats, fruits, and vegetables. This helps regulate blood sugar levels.
- Carbohydrate Counting: Learning to count carbohydrates can help manage insulin doses effectively.
- Portion Control: Be mindful of portion sizes to prevent overeating and avoid significant blood sugar fluctuations.
- Regular Physical Activity
- Exercise: Engage in at least 150 minutes of moderate aerobic activity each week, such as walking, swimming, or cycling. Regular physical activity helps increase insulin sensitivity and lower blood sugar levels.
- Strength Training: Incorporate resistance exercises at least twice a week to build muscle and improve metabolic health.
- Blood Sugar Monitoring
- Regular Monitoring: Use a glucometer to check blood sugar levels regularly. Keeping track helps identify patterns and informs necessary adjustments to diet or insulin doses.
- Continuous Glucose Monitoring (CGM): Some individuals may benefit from CGM devices that provide real-time blood glucose readings.
- Managing Hypoglycemia
- Recognizing Low Blood Sugar: Symptoms include shaking, sweating, irritability, and confusion.
- Emergency Treatment: Always carry fast-acting carbohydrates, like glucose tablets or juice, to treat hypoglycemia quickly.
- Stress Management
- Mindfulness Techniques: Practices such as yoga, meditation, and deep-breathing exercises can help reduce stress, which can negatively affect blood sugar levels.
- Adequate Sleep: Prioritize good sleep hygiene, as poor sleep can lead to insulin resistance and unstable blood sugar levels.
- Education and Support
- Diabetes Education: Attend diabetes education programs to learn about managing the condition effectively.
- Support Groups: Connecting with others living with Type 1 diabetes can provide emotional support and practical advice.
Tips for Living Well with Type 1 Diabetes
- Stay Hydrated: Drink plenty of water to help flush out excess glucose and stay hydrated.
- Meal Planning: Prepare meals ahead of time to ensure balanced nutrition and avoid unhealthy choices.
- Read Nutrition Labels: Learn to read food labels to make informed decisions about carbohydrate intake.
- Regular Foot Care: Inspect feet daily for cuts, blisters, or sores, and seek medical advice if issues arise.
- Keep Emergency Supplies: Always have a supply of fast-acting carbohydrates on hand to treat low blood sugar episodes.
Psychological Aspects of Type 1 Diabetes
Living with Type 1 diabetes can be challenging, both physically and emotionally. It’s essential to recognize the psychological aspects:
- Mental Health: Many individuals with diabetes experience anxiety, depression, or diabetes distress. Seeking support from mental health professionals or joining support groups can be beneficial.
- Diabetes Burnout: The constant management of diabetes can lead to burnout. It’s important to communicate openly with healthcare providers and consider adjustments to the treatment plan when feeling overwhelmed.
Conclusion
Type 1 diabetes is a lifelong condition that requires diligent management and lifestyle adjustments. Understanding the symptoms and potential complications is essential for effective control. By implementing a comprehensive strategy that includes insulin therapy, a balanced diet, regular exercise, and consistent monitoring, individuals with Type 1 diabetes can lead fulfilling lives while minimizing the risk of complications. Always consult healthcare professionals for personalized advice and treatment options tailored to individual needs. With the right tools and support, it is possible to thrive while living with Type 1 diabetes.